See also
Acute red eye
Acute eye injury
Penetrating eye injury
Periorbital cellulitis
Key points
- Assessing visual acuity can be difficult but should be performed early (before examination when the child may become distressed)
- Visual acuity is assessed for each eye based on the child’s age and ability to interact
- Adequate analgesia will aid examination and procedural sedation may be required in the younger child
- Fluorescein shows corneal abnormalities when viewed under cobalt blue light. Stain with fluorescein if corneal abrasion, ulcer or foreign body is suspected
- Serious periocular trauma should be treated as a suspected ruptured or penetrated globe and managed by minimising distress, placing an eye shield and urgently referring to ophthalmology, see
Penetrating eye injury
Background
- Assessment of the eye and vision can be very difficult in children, particularly if the child is injured or distressed
- Eye drops (except fluorescein) sting. Topical anaesthetic eye drops, although initially painful, can be very useful as it will relieve pain for about 20 minutes and may allow the child to spontaneously open their eye after a couple of minutes
- Key features of sight threatening conditions are severe eye pain, photophobia, decreased visual acuity or a history of possible penetrating eye trauma
- It is usually not necessary to dilate a child’s pupils in emergency for assessment and should not be done in situations of head injury or trauma
Assessment
- A lot of information can be gathered by initially observing the child (eg eye red or white, cellulitis or swelling of eyelids, ptosis, proptosis, eye movements, cranial nerve palsy)
- Adequate analgesia will aid assessment and procedural sedation may be required in the younger child
- Topical anaesthetic such as tetracaine (amethocaine) 0.5% or 1% can be used to assist with examination
- One drop into the affected eye will induce anaesthesia after 20 seconds and the effect lasts 10 – 20 minutes (longer with 1%)
- Avoid repeated administration of anaesthetic eye drops due to direct epithelial toxicity that can delay corneal healing
Examination
Essential components of examination and the order in which they should be performed are:
- Visual acuity (and visual fields if there is visual loss/change)
- General inspection
- Pupils
- Look for pupillary light reflex (direct and consensual response for each eye), pupil shape and size, symmetry with other eye
- Red reflex with direct ophthalmoscope
- The reflex is missing if the retina is detached or there is an opacity at the cornea, anterior chamber, lens and vitreous
Additional components are:
- Slit lamp examination
- Examine the conjunctiva, pupil, iris and cornea using a slit lamp whenever possible
- Examination with direct ophthalmoscope
- Cranial nerves
Visual acuity
- Assessing visual acuity can be difficult but should be performed early (before examination when the child may become distressed). Enlist the parent’s help for covering an eye or holding a visual target
- Visual acuity is assessed for each eye based on the child’s age and ability to interact:
- From 5 years or older: Snellen chart
- From 3 – 5 years: ‘Tumbling E’ eye chart
- From 2 – 3 years: Kay picture book, ability to identify and reach for a small, coloured target (like single 100s and 1000s or similarly sized rolled up pieces of paper)
-
<2 – 3 years: fix and follow light and blinks to bright lights. Looks at a target with central, steady and maintained gaze
- A difference of greater than 2 lines (on an eye chart) between the eyes is likely to be significant
Visual fields
- Four quadrant confrontation testing in each eye in older children
- Traumatic visual field loss is usually gross, however subtle changes may occasionally occur with retinal detachment and intraocular foreign body
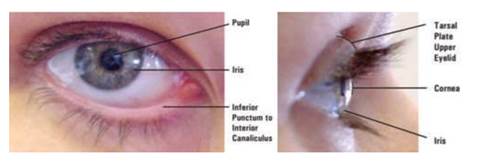
External anatomy of the eye
General Inspection
- Does the eye look intact? Are there periocular injuries or injury to globe?
- Is the eye red or white? Is the redness localised or diffuse?
- Is the condition unilateral or bilateral?
- Any ptosis, proptosis or misalignment of the eye?
- Is there a retrobulbar haemorrhage? Bulging, tense, proptotic eye with inability to close the eyelids following blunt trauma, see
Acute eye injury and
Penetrating eye injury
- Is there cellulitis or swelling of the eyelids or skin around the eye? See
Periorbital cellulitis
- Are there periocular lacerations or ecchymoses?
- Is there a cranial nerve palsy?
Eye movements
- Assess both eyes first, then each eye separately
- Check the child can look in all directions. When testing eye movements, it may help to gently place a finger on the child’s chin or forehead to remind them not to follow with their head
- Check for diplopia or pain with eye movement
- Exclude entrapment of extraocular muscles with orbital fractures
Eyelids, conjunctiva and sclera
- Assess for redness or swelling of eyelids. Is the swelling involving the tarsal conjunctiva?
- Observe for ptosis (compare the position of the upper eyelid on one side with the other). Assess for weakness (gently trying to part closed eyelids)
- Examine the lids including everting the eyelids for trauma and foreign bodies. A topical anaesthetic may aid examination or procedural sedation may be required in younger children
- To evert the eyelid:
- Ask the child to look down
- Gently pull the upper eyelid down and away from the globe using the eyelashes
- Place a cotton bud at the midpoint on top of the eyelid, then bend the eyelid up over the cotton bud (during this last step, slide the cotton bud out and either replace it on the lid margin to hold the lid in position or use your finger to do so)
Cornea, anterior chamber, iris and pupil
- If the cornea is affected, the child will often be reluctant to open their eye
- Before fluorescein: Look for pupillary light reflex, pupil shape and size, symmetry with other eye, assess for a Relative Afferent Pupillary Defect, presence of hyphaema or cloudy cornea (prior to blood settling), or epithelial defects
- If using fluorescein apply 1 drop to each eye, or for strips – wet strip with 0.9% sodium chloride and touch to lower lid only
- After fluorescein: Look for corneal, conjunctival abrasions or lacerations
- Look for vertically-linear corneal abrasions, as these particularly suggest a foreign body under the upper-lid
Fundus
- Using a direct ophthalmoscope look for red reflex, assess optic disc, the macula and periphery
- Vitreous haemorrhage can cause diminished red reflex, difficulty visualising fundus or red splotches on retina
- Retinal detachment may be seen as a grey flap out of focus with optic disc on direct ophthalmoscopy
- Check for retinal haemorrhages and papilloedema
Palpate the orbital rim
- Assess for bony fractures
Consider consultation with local paediatric team when
Any child with suspected child abuse, suspected STI-related conjunctivitis, or possible systemic illness
Consider consultation with ophthalmology when:
- A child with suspected sight threatening condition
- If required to facilitate a complete examination particularly in distressed child
- If retinal assessment and photography is required for suspected child abuse
Consider transfer when
- A child with a sight threatening condition and/or management is beyond the capacity of the local team
- To facilitate ophthalmological assessment
For emergency advice and paediatric or neonatal ICU transfers, see
Retrieval
Services
Additional notes
The
Eye Emergency Manual App provides clinical guidelines for the management of eye emergencies and provides a ‘paediatric filter’
Last updated October 2022